In the advantages administration {industry}, claims processing is a crucial operational pillar that makes positive workers and beneficiaries obtain well timed advantages, akin to well being, dental, or incapacity funds, whereas controlling prices and adhering to laws like HIPAA and ERISA. Companies goal to optimize the workflow—masking declare submission, validation, adjudication, cost, and appeals—to reinforce worker satisfaction, strengthen supplier relationships, and mitigate monetary dangers. The method consists of particular steps like declare submission (by way of portals or paper), information validation (verifying eligibility and accuracy), adjudication (assessing protection towards plan guidelines), cost or denial (together with test processing for reimbursements), and attraction dealing with. Environment friendly claims processing helps aggressive advantages choices, which is essential for expertise retention and employer branding, however requires balancing velocity, accuracy, and price in a extremely regulated atmosphere.
Regardless of its significance, claims processing faces important challenges in lots of organizations. Most notably, the reliance on legacy programs and guide processes leads to frustratingly sluggish decision instances, excessive error charges, and elevated administrative prices. Incomplete or inaccurate declare submissions—akin to these with lacking analysis codes or eligibility mismatches—incessantly result in denials and rework, creating frustration for each workers and healthcare suppliers. Moreover, fraud, waste, and abuse proceed to inflate prices, but detecting these points with out delaying respectable claims stays difficult. Advanced regulatory necessities demand fixed system updates, and poor integration between programs—akin to Human Useful resource Info Techniques (HRIS) and different downstream programs—severely limits scalability. These points drive up operational bills, erode belief in advantages packages, and overburden customer support groups, significantly throughout appeals processes or peak claims intervals.
Generative AI may also help handle these challenges. With Amazon Bedrock Information Automation, you’ll be able to automate era of helpful insights from unstructured multimodal content material akin to paperwork, photos, audio, and video. Amazon Bedrock Information Automation can be utilized in advantages claims course of to automate doc processing by extracting and classifying paperwork from claims packets, coverage functions, and supporting paperwork with industry-leading accuracy, decreasing guide errors and accelerating decision instances. Amazon Bedrock Information Automation pure language processing capabilities interpret unstructured information, akin to supplier notes, supporting compliance with plan guidelines and laws. By automating repetitive duties and offering insights, Amazon Bedrock Information Automation helps cut back administrative burdens, improve experiences for each workers and suppliers, and assist compliance in a cheap method. Moreover, its scalable structure permits seamless integration with present programs, enhancing information move throughout HRIS, claims programs, and supplier networks, and superior analytics assist detect fraud patterns to optimize value management.
On this publish, we study the standard profit claims processing workflow and determine the place generative AI-powered automation can ship the best influence.
Profit claims processing
When an worker or beneficiary pays out of pocket for an expense coated underneath their well being advantages, they submit a declare for reimbursement. This course of requires a number of supporting paperwork, together with physician’s prescriptions and proof of cost, which could embody test photos, receipts, or digital cost confirmations.
The claims processing workflow entails a number of vital steps:
- Doc consumption and processing – The system receives and categorizes submitted documentation, together with:
- Medical data and prescriptions
- Proof of cost documentation
- Supporting types and eligibility verification
- Fee verification processing – For check-based reimbursements, the system should full the next steps:
- Extract data from test photos, together with the account quantity and routing quantity contained within the MICR line
- Confirm payee and payer names towards the data offered throughout the declare submission course of
- Verify cost quantities match the claimed bills
- Flag discrepancies for human overview
- Adjudication and reimbursement – When verification is full, the system performs a number of actions:
- Decide eligibility primarily based on plan guidelines and protection limits
- Calculate acceptable reimbursement quantities
- Provoke cost processing by way of direct deposit or test issuance
- Present notification to the claimant concerning the standing of their reimbursement
On this publish, we stroll by way of a real-world state of affairs to make the complexity of this multi-step course of clearer. The next instance demonstrates how Amazon Bedrock Information Automation can streamline the claims processing workflow, from preliminary submission to last reimbursement.
Resolution overview
Let’s think about a state of affairs the place a profit plan participant seeks remedy and pays out of pocket for the physician’s charge utilizing a test. They then purchase the medicines prescribed by the physician on the pharmacy retailer. Later, they log in to their profit supplier’s portal and submit a declare together with the picture of the test and cost receipt for the medicines.
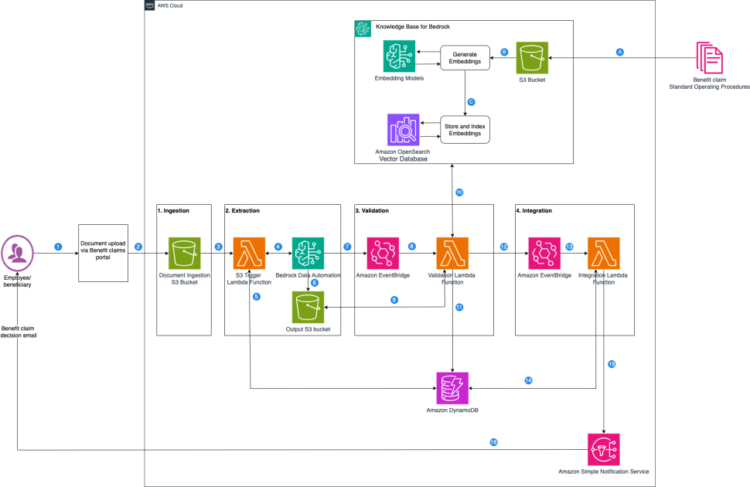
This answer makes use of Amazon Bedrock Information Automation to automate the 2 most crucial and time-consuming elements of this workflow: doc consumption and cost verification processing. The next diagram illustrates the advantages claims processing structure.

The top-to-end course of works by way of 4 built-in levels: ingestion, extraction, validation, and integration.
Ingestion
When a beneficiary uploads supporting paperwork (test picture and pharmacy receipt) by way of the corporate’s profit claims portal, these paperwork are securely saved in an Amazon Easy Storage Service (Amazon S3) bucket, triggering the automated claims processing pipeline.
Extraction
After paperwork are ingested, the system instantly begins with clever information extraction:
- The S3 object add triggers an AWS Lambda operate, which invokes the Amazon Bedrock Information Automation venture.
- Amazon Bedrock Information Automation makes use of blueprints for file processing and extraction. Blueprints are artifacts used to configure file processing enterprise logic by specifying a listing of discipline names for information extraction, together with their desired information codecs (string, quantity, or Boolean) and pure language context for information normalization and validation guidelines. Amazon Bedrock Information Automation gives a catalog of pattern blueprints out of the field. You’ll be able to create a customized blueprint on your distinctive doc varieties that aren’t predefined within the catalog. This answer makes use of two blueprints designed for various doc varieties, as proven within the following screenshot:
- The catalog blueprint
US-Financial institution-Testfor test processing. - The customized blueprint
benefit-claims-pharmacy-receipt-blueprintfor pharmacy-specific receipts.
- The catalog blueprint

US-Financial institution-Test is a catalog blueprint offered out of the field by Amazon Bedrock Information Automation. The customized blueprint benefit-claims-pharmacy-receipt-blueprint is created utilizing an AWS CloudFormation template to deal with pharmacy receipt processing, addressing a selected doc sort that wasn’t out there in the usual blueprint catalog. The profit administrator desires to search for vendor-specific data akin to title, handle, and cellphone particulars for advantages claims processing. The customized blueprint schema incorporates pure language clarification of these fields, akin to VendorName, VendorAddress, VendorPhone, and extra fields, explaining what the sphere represents, anticipated information varieties, and inference sort for every extracted discipline (defined in Creating Blueprints for Extraction), as proven within the following screenshot.

3. The 2 blueprints are added to the Amazon Bedrock Information Automation venture. An Amazon Bedrock Information Automation venture is a grouping of each commonplace and customized blueprints that you should use to course of various kinds of recordsdata (like paperwork, audio, and pictures) utilizing particular configuration settings, the place you’ll be able to management what sort of data you wish to extract from every file sort. When the venture is invoked asynchronously, it mechanically applies the suitable blueprint, extracts data akin to confidence scores and bounding field particulars for every discipline, and saves leads to a separate S3 bucket. This clever classification alleviates the necessity so that you can write advanced doc classification logic.
The next screenshot illustrates the doc classification by the usual catalog blueprint US-Financial institution-Test.

The next screenshot exhibits the doc classification by the customized blueprint benefit-claims-pharmacy-receipt-blueprint.

Validation
With the info extracted, the system strikes to the validation and decision-making course of utilizing the enterprise guidelines particular to every doc sort.
The enterprise guidelines are documented in commonplace working process paperwork (AnyCompany Profit Checks Normal Working process.docx and AnyCompany Profit Claims Normal Working process.docx) and uploaded to an S3 bucket. Then the system creates a information base for Amazon Bedrock with the S3 bucket because the supply, as proven within the following screenshot.

When the extracted Amazon Bedrock Information Automation outcomes are saved to the configured S3 bucket, a Lambda operate is triggered mechanically. Based mostly on the enterprise guidelines retrieved from the information base for the precise doc sort and the extracted Amazon Bedrock Information Automation output, an Amazon Nova Lite giant langue mannequin (LLM) makes the automated approve/deny resolution for claims.
The next screenshot exhibits the profit declare adjudication automated resolution for US-Financial institution-Test.

The next screenshot exhibits the profit declare adjudication automated resolution for benefit-claims-pharmacy-receipt-blueprint.

Integration
The system seamlessly integrates with present enterprise processes.
When validation is full, an occasion is pushed to Amazon EventBridge, which triggers a Lambda operate for downstream integration. On this implementation, we use an Amazon DynamoDB desk and Amazon Easy Notification Service (Amazon SNS) e mail for downstream integration. A DynamoDB desk is created as a part of the deployment stack, which is used to populate particulars together with doc classification, extracted information, and automatic resolution. An e mail notification is distributed for each test and receipts after the ultimate resolution is made by the system. The next screenshot exhibits an instance e mail for pharmacy receipt approval.

This versatile structure helps you combine along with your present functions by way of inner APIs or occasions to replace declare standing or set off extra workflows when validation fails.
Lowering guide effort by way of clever enterprise guidelines administration
Past automating doc processing, this answer addresses a standard operational problem: Historically, prospects should write and preserve code for dealing with enterprise guidelines round claims adjudication and processing. Each enterprise rule change requires growth effort and code updates, slowing time-to-market and growing upkeep overhead.
Our strategy converts enterprise guidelines and commonplace working procedures (SOPs) into information bases utilizing Amazon Bedrock Data Bases, which you should use for automated decision-making. This strategy can dramatically cut back time-to-market when enterprise guidelines change, as a result of updates could be made by way of information administration slightly than code deployment.
Within the following sections, we stroll you thru the steps to deploy the answer to your individual AWS account.
Conditions
To implement the answer offered on this publish, you have to have the next:
This answer makes use of Python 3.13 with Boto3 1.38. or later model, and the AWS Serverless Software Mannequin Command Line Interface (AWS SAM CLI) model 1.138.0. We assume that you’ve put in these in your native machine already. If not, seek advice from the next directions:
Arrange code in your native machine
To arrange the code, clone the GitHub repository. After you’ve got cloned the repository to your native machine, the venture folder construction will appear like the next code, as talked about within the README file:

Deploy the answer in your account
The pattern code comes with a CloudFormation template that creates needed sources. To deploy the answer in your account, observe the deployment directions within the README file.
Clear up
Deploying this answer in your account will incur prices. Comply with the cleanup directions within the README file to keep away from costs if you find yourself carried out.
Conclusion
Advantages administration firms can considerably improve their operations by automating claims processing utilizing the answer outlined on this publish. This strategic strategy immediately addresses the {industry}’s core challenges and may ship a number of key benefits:
- Enhanced processing effectivity by way of accelerated claims decision instances, diminished guide error charges, and better straight-through processing charges that decrease the irritating delays and guide rework plaguing legacy programs
- Streamlined doc integration and fraud detection capabilities, the place including new supporting paperwork turns into seamless by way of new Amazon Bedrock Information Automation blueprints, whereas AI-powered analytics determine suspicious patterns with out delaying respectable claims, avoiding conventional months-long growth cycles and decreasing expensive fraud, waste, and abuse
- Agile enterprise rule administration that permits fast adaptation to altering HIPAA and ERISA necessities and modification of enterprise guidelines, considerably decreasing administrative prices and time-to-market whereas enhancing scalability and integration with present HRIS and claims, in the end enhancing worker satisfaction, strengthening supplier relationships, and supporting aggressive advantages choices which might be essential for expertise retention and employer branding
To get began with this answer, seek advice from the GitHub repo. For extra details about Amazon Bedrock Information Automation, seek advice from Remodel unstructured information into significant insights utilizing Amazon Bedrock Information Automation and check out the Doc Processing Utilizing Amazon Bedrock Information Automation workshop.
Concerning the authors
 Saurabh Kumar is a Senior Options Architect at AWS primarily based out of Raleigh, NC, with experience in Resilience Engineering, Chaos Engineering, and Generative AI options. He advises prospects on fault-tolerance methods and generative AI-driven modernization approaches, serving to organizations construct strong architectures whereas leveraging generative AI applied sciences to drive innovation.
Saurabh Kumar is a Senior Options Architect at AWS primarily based out of Raleigh, NC, with experience in Resilience Engineering, Chaos Engineering, and Generative AI options. He advises prospects on fault-tolerance methods and generative AI-driven modernization approaches, serving to organizations construct strong architectures whereas leveraging generative AI applied sciences to drive innovation.
 Kiran Lakkireddy is a Principal Options Architect at AWS with experience in Monetary Providers, Advantages Administration and HR Providers industries. Kiran gives expertise and structure steerage to prospects of their enterprise transformation, with a specialised deal with GenAI safety, compliance, and governance. He frequently speaks to buyer safety management on GenAI safety, compliance, and governance subjects, serving to organizations navigate the advanced panorama of AI implementation whereas sustaining strong safety requirements.
Kiran Lakkireddy is a Principal Options Architect at AWS with experience in Monetary Providers, Advantages Administration and HR Providers industries. Kiran gives expertise and structure steerage to prospects of their enterprise transformation, with a specialised deal with GenAI safety, compliance, and governance. He frequently speaks to buyer safety management on GenAI safety, compliance, and governance subjects, serving to organizations navigate the advanced panorama of AI implementation whereas sustaining strong safety requirements.
 Tamilmanam Sambasivam is a Options Architect and AI/ML Specialist at AWS. She helps enterprise prospects to unravel their enterprise issues by recommending the appropriate AWS options. Her sturdy again floor in Info Expertise (24+ years of expertise) helps prospects to strategize, develop and modernize their enterprise issues in AWS cloud. Within the spare time, Tamil prefer to journey and gardening.
Tamilmanam Sambasivam is a Options Architect and AI/ML Specialist at AWS. She helps enterprise prospects to unravel their enterprise issues by recommending the appropriate AWS options. Her sturdy again floor in Info Expertise (24+ years of expertise) helps prospects to strategize, develop and modernize their enterprise issues in AWS cloud. Within the spare time, Tamil prefer to journey and gardening.